|
HAM711S - HAEMATOLOGY 3 - 2ND OPP - JULY 2023 |
 |
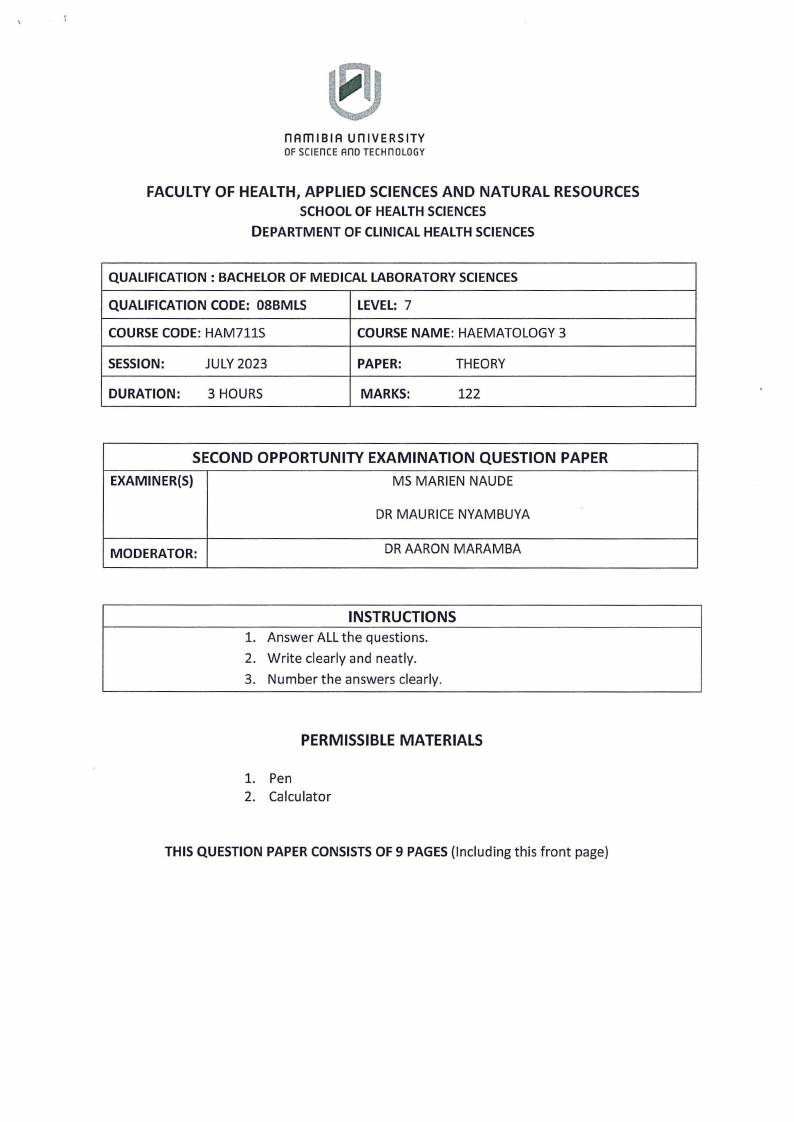
1 Page 1 |
▲back to top |
 |
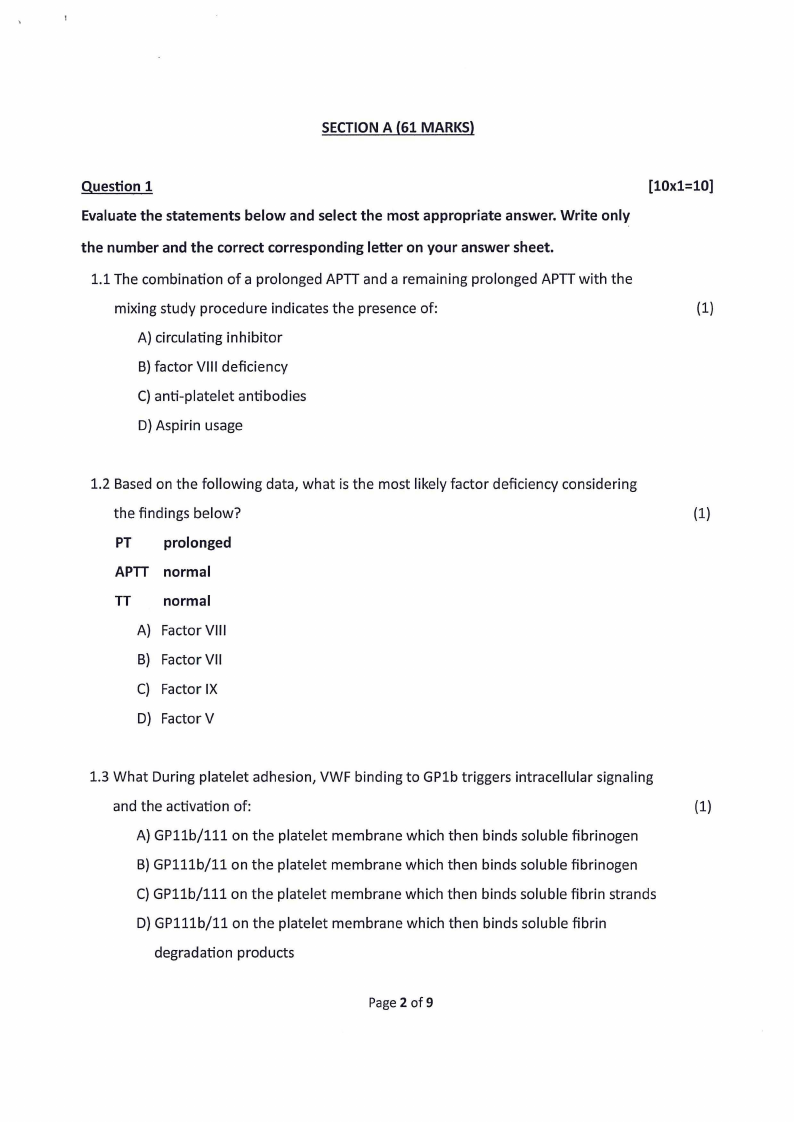
2 Page 2 |
▲back to top |
 |
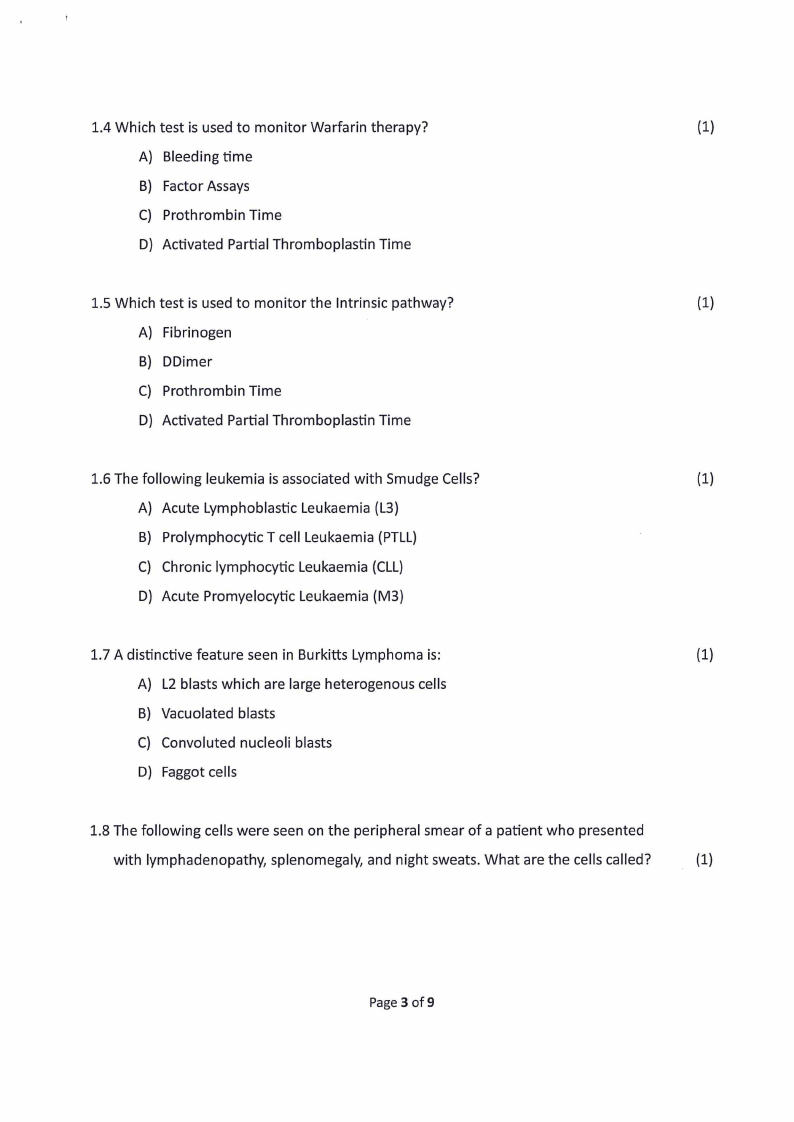
3 Page 3 |
▲back to top |
 |
4 Page 4 |
▲back to top |
 |
5 Page 5 |
▲back to top |
 |
6 Page 6 |
▲back to top |
 |
7 Page 7 |
▲back to top |
 |
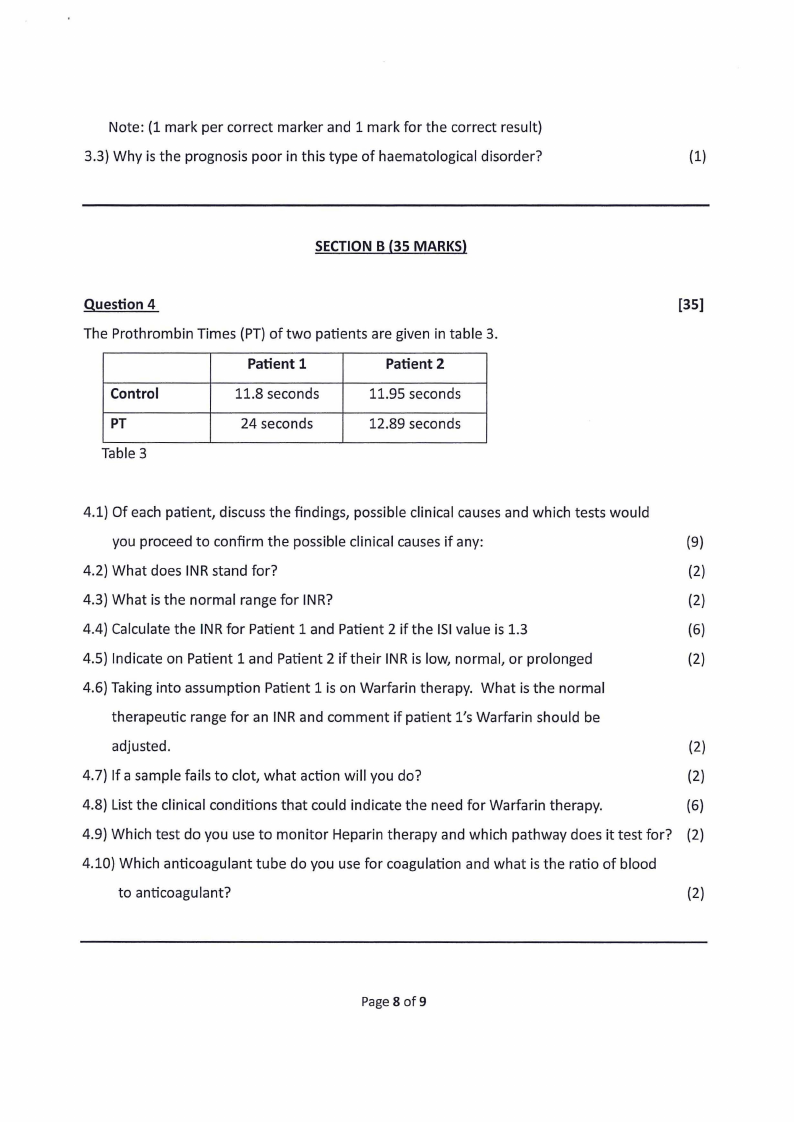
8 Page 8 |
▲back to top |
 |
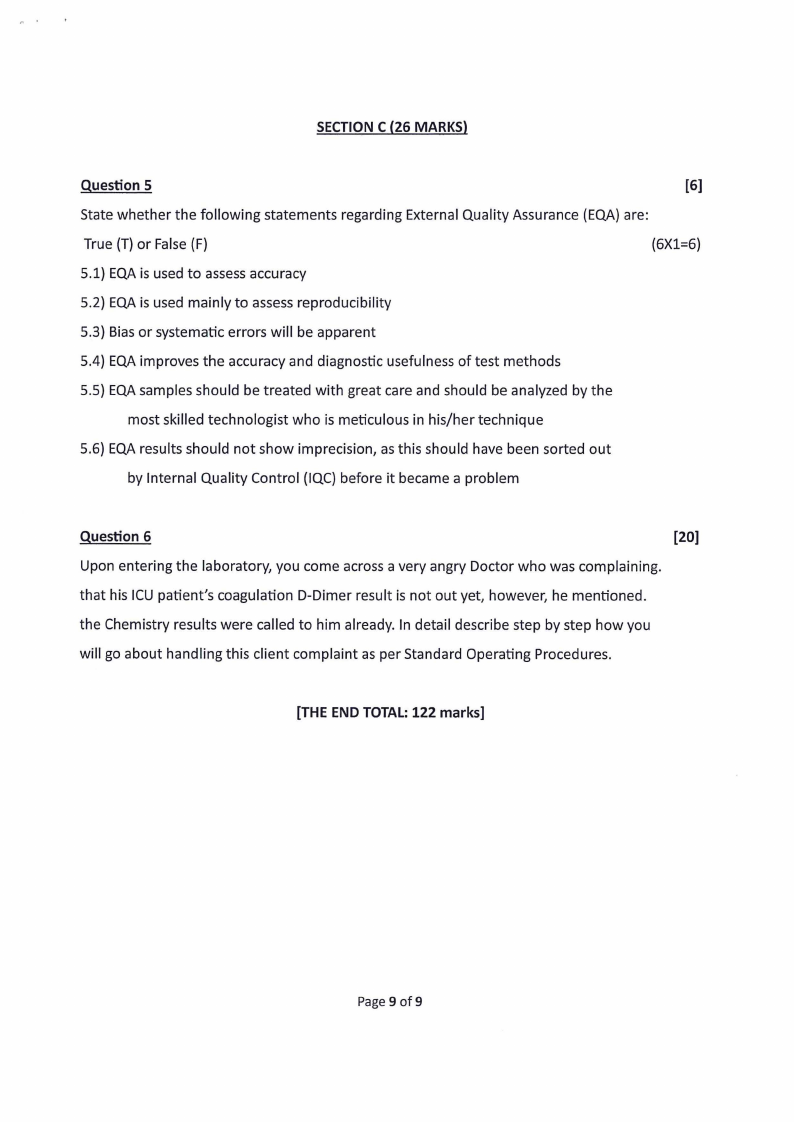
9 Page 9 |
▲back to top |