 |
ICP811S - INTERGRATED CLINICAL PATHOPHYSIOLOGY - 2ND OPP - JULY 2022 |
 |
1 Page 1 |
▲back to top |
nAm I BIA un IVERS ITY
OF SCIEn CE Ano TECHn OLOGY
FACULTYOF HEALTH,APPLIEDSCIENCESAND NATURALRESOURCES
DEPARTMENTOF HEALTHSCIENCES
QUALIFICATION: BACHELORMEDICAL LABORATORYSCIENCES
QUALIFICATION CODE: 08BMLS
LEVEL: 8
COURSENAME: INTEGRATEDCLINICALPATHOPHYSIOLOGY COURSECODE: ICP811S
SESSION:JULY 2022
DURATION: 3 HOURS
PAPER:THEORY
MARKS: 140
SUPPLEMENTARY/SECONDOPPORTUNITYEXAMINATION PAPER
EXAMINER(S) Ms Roselin Tsauses, Mrs Fredrika Engelbrecht, Dr Maurice Nyambuya, Dr
Munyaradzi Mukesi
MODERATOR: Prof Glenda Davison
INSTRUCTIONS
1. Answer ALL the questions.
2. Write clearly and neatly.
3. Number the answers clearly.
PERMISSIBLEMATERIALS
1. Pen
2. Calculator
THIS QUESTION PAPERCONSISTSOF 7 PAGES(including this front page)
1
 |
2 Page 2 |
▲back to top |
SECTIONA [70]
QUESTION 1
[5]
1.0 Review the patient results below and enumerate the following:
PATIENT RESULTS
Na
146 mmol/L
K
9.1 mmol/L
Cl
97 mmol/L
CO2
23 mmol/L
Urea
39.8 mmol/L
Creatinine
1112 µmol/L
Total calcium
1.65 mmol/L
Fe
19.7µmol/L
Transferin
3.56g/L
Total protein
83g/L
Albumin
32g/L
Glucose
19.5 mmol/L
Cholesterol
4.7 mmol/L
Triglyceride
3.38 mmol/L
HDL
1.1 mmol/L
1.1 Osmolality
(1)
1.2 % Transferin saturation
(2)
1.3 Corrected calcium
(1)
1.4 LDL
(1)
QUESTION 2
[S]
A critical patient's blood gas results are as follows:
Blood gas results
7.21
(7.35-7.45)
61 mmHg (35-45)
64 mmHg (75-100)
24 mmol/L (22-26)
2.1 Select THREEimportant transport related requirements for blood gas samples. (2)
2.2 Showing all steps, determine the acid base and compensation status of the
patient above.
(3)
2
 |
3 Page 3 |
▲back to top |
QUESTION 3
[10]
Using the thyroid gland as an example, explain the following methods of hormone
assessment:
3.1 Direct static
(2)
3.2 Direct dynamic
(4)
3.3 Indirect
(4)
QUESTION 4
[10]
4.1 State the recommended order of blood draw for plastic vacutainer tubes.
(2)
4.2 Is heparin recommended for coagulation and haematology testing? Motivate
your answer.
(2)
4.3 Is the ratio of anticoagulant to blood critical? Motivate your answer.
(2)
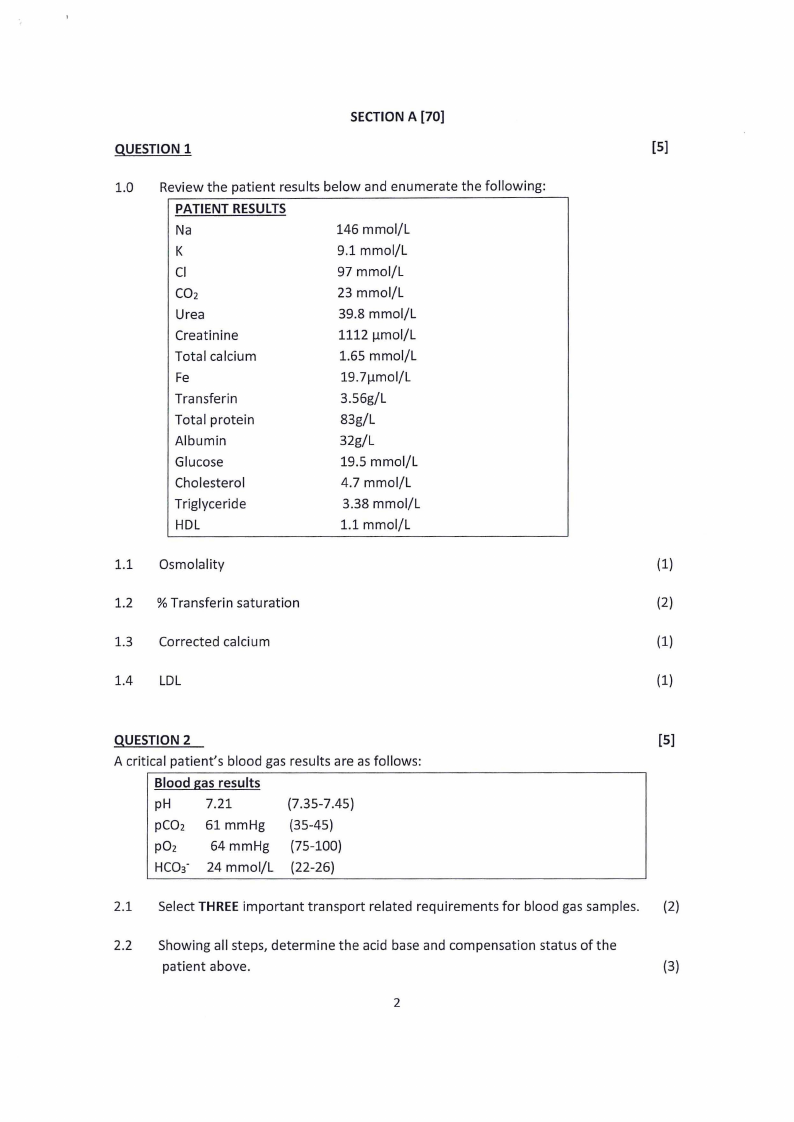
4.4 The picture below illustrates an in vitro effect of EDTAon a blood smear.
Name and describe this phenomenon.
(4)
QUESTION 5
State the Coulter principle and describe its use in haematology automation.
[10]
(10)
QUESTION 6
[20]
A 7 years old scholar was admitted into Red Cross children hospital with a high fever
and vomiting. She presented with severe headache and was unable to bend her neck.
A preliminary diagnosis of meningitis was made. Cerebrospinal fluid was taken and the
following cell count was reported 250 White blood cells predominately Polymorph
nuclear cells, chemistry results: Protein: >200mg/dl (ref 50-80mg/dl), Glucose <40
(ref 70-80mg/dL)
3
 |
4 Page 4 |
▲back to top |
6.1 Which type of meningitis do you think this patient has?
(1)
6.2 Mention the microorganisms that are normally associated with neonatal
meningitis.
(3)
6.3 After the CSFwas cultured, a gram stain was performed and gram negative
diplococci were observed. Which is the most likely microorganism involved?
(1)
6.4 How would you differentiate between the two species of microorganisms
involved?
(5)
6.5 Discussthe pathogenesis of the microorganism involved.
(10)
QUESTION 7
[10]
A 20-year-old woman, with a 22-year-old partner who has a provisional diagnosis of
gonorrhoea (confirmed by the lab), visits a physician even though she does not have any
pain or vaginal irritation. On physical examination, the woman has greenish discharge
emanating from the mouth of her cervix. Her cervix is inflamed and bleeds easily when
a swab is used to remove adherent secretions. Her male partner had a purulent discharge
from his penis for the past 2 days and was given antibiotics by his first physician. He now
notices a milder but persistent urethral discharge and dysuria. Gram stains from both
patients reveal numerous neutrophils, but no evidence of Gram-negative diplococci.
7.1 What is your preliminary diagnosis of both patient's condition and what
laboratory test(s) would you order to confirm it?
(3)
7.2 What are the possible causative agents of this disease?
(3)
7.3 What type of samples should be taken to confirm your diagnosis?
(4)
SECTION B [70]
QUESTION 8
[40]
A 66 year old male with known CLLis admitted to ICUwith severe lung infection
and pleural effusion. Blood, sputum and pleural fluid samples are submitted to
the laboratory for analysis. The following are some of the results obtained:
4
 |
5 Page 5 |
▲back to top |
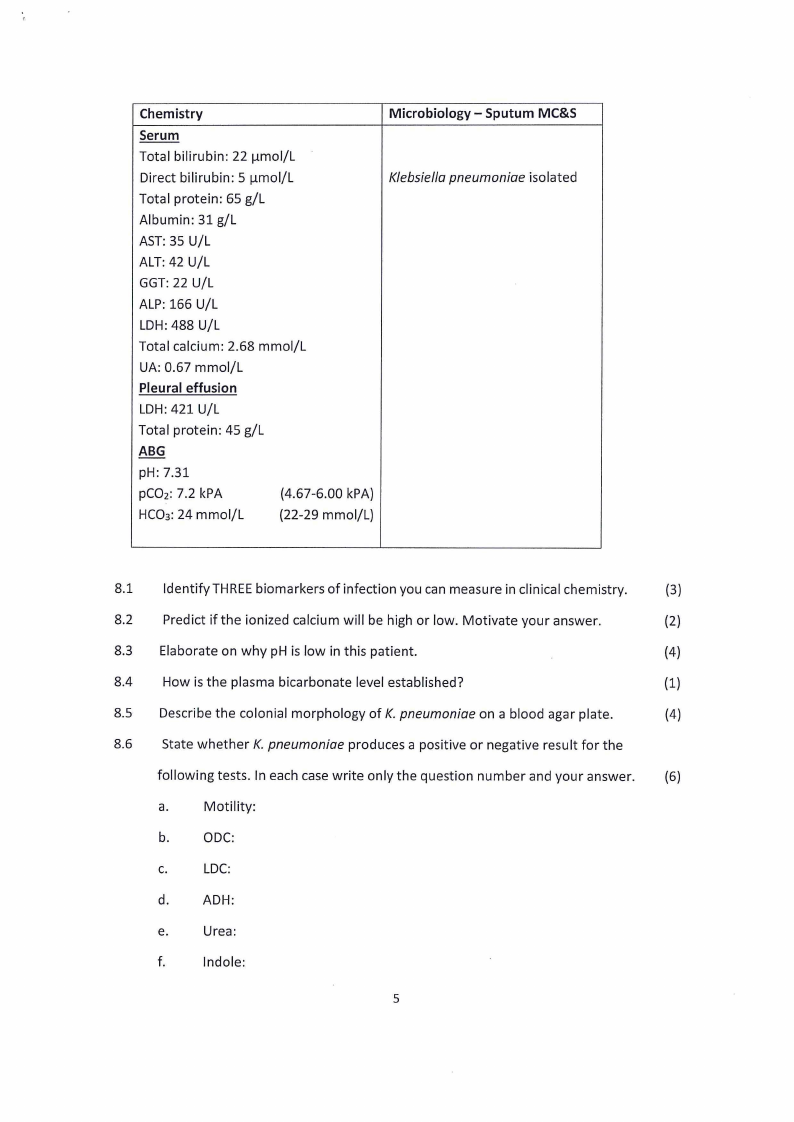
Chemistry
Serum
Total bilirubin: 22 µmol/L
Direct bilirubin: 5 µmol/L
Total protein: 65 g/L
Albumin: 31 g/L
AST: 35 U/L
ALT: 42 U/L
GGT: 22 U/L
ALP: 166 U/L
LDH: 488 U/L
Total calcium: 2.68 mmol/L
UA: 0.67 mmol/L
Pleural effusion
LDH: 421 U/L
Total protein: 45 g/L
ABG
pH: 7.31
pC02: 7.2 kPA
(4.67-6.00 kPA)
HC03: 24 mmol/L
(22-29 mmol/L)
Microbiology - Sputum MC&S
Klebsiella pneumoniae isolated
8.1 Identify THREEbiomarkers of infection you can measure in clinical chemistry.
(3)
8.2 Predict if the ionized calcium will be high or low. Motivate your answer.
(2)
8.3 Elaborate on why pH is low in this patient.
(4)
8.4 How is the plasma bicarbonate level established?
(1)
8.5 Describe the colonial morphology of K. pneumoniae on a blood agar plate.
(4)
8.6 State whether K. pneumoniae produces a positive or negative result for the
following tests. In each case write only the question number and your answer. (6)
a.
Motility:
b.
ODC:
C.
LDC:
d.
ADH:
e.
Urea:
f.
lndole:
5
 |
6 Page 6 |
▲back to top |
8.7 Briefly explain the pathogenesis of aplastic anaemia.
(2)
8.8 Explain why infections may lead to the development of aplastic anaemia.
(3)
8.9 Discuss the morphology characteristically observed on the bone marrow
and peripheral blood smear of a patient with aplastic anaemia.
(5)
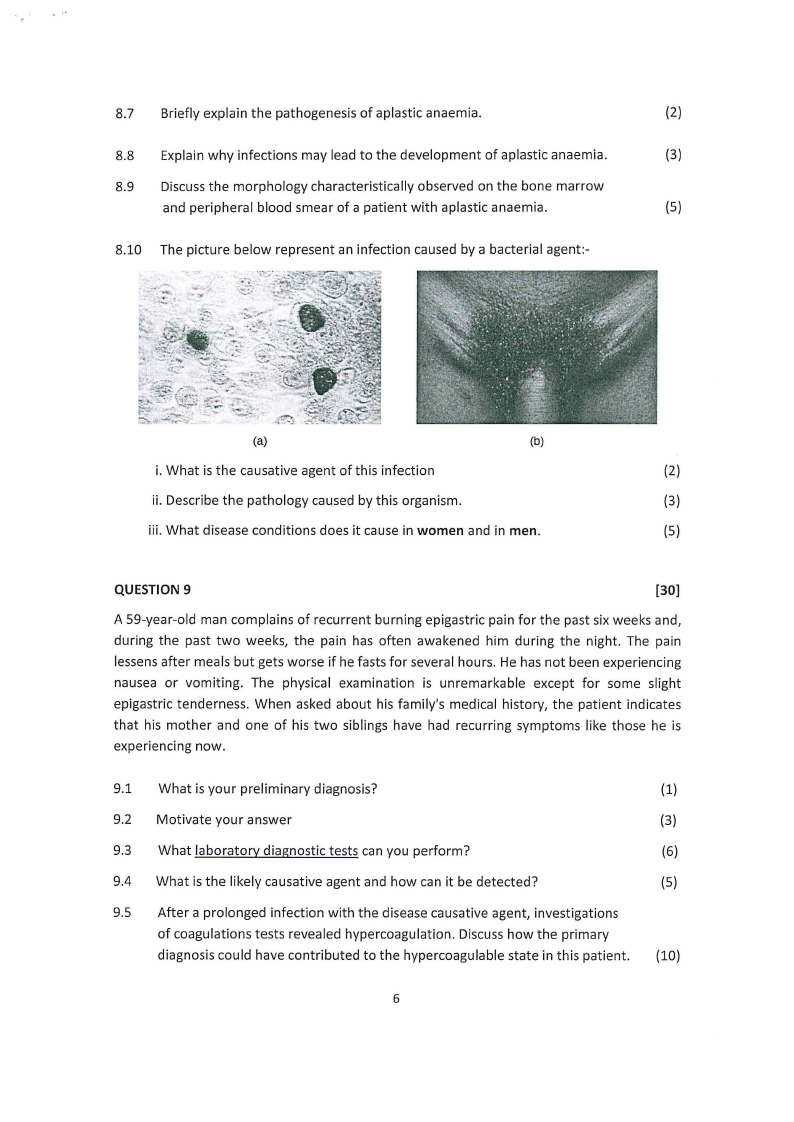
8.10 The picture below represent an infection caused by a bacterial agent:-
..
:----: _,,.
.
t',,.;>° --~'-·
;;,
.....
./...._,,,~..
,.,.. "4
,. =~it\\~,--~;~-;t, "',~"
~,
~J
....
~'ty~•''r,_
(a)
(b)
i. What is the causative agent of this infection
(2)
ii. Describe the pathology caused by this organism.
(3)
iii. What disease conditions does it cause in women and in men.
(5)
QUESTION 9
[30]
A 59-year-old man complains of recurrent burning epigastric pain for the past six weeks and,
during the past two weeks, the pain has often awakened him during the night. The pain
lessens after meals but gets worse if he fasts for several hours. He has not been experiencing
nausea or vomiting. The physical examination is unremarkable except for some slight
epigastric tenderness. When asked about his family's medical history, the patient indicates
that his mother and one of his two siblings have had recurring symptoms like those he is
experiencing now.
9.1 What is your preliminary diagnosis?
(1)
9.2 Motivate your answer
(3)
9.3 What laboratory diagnostic tests can you perform?
(6)
9.4 What is the likely causative agent and how can it be detected?
(5)
9.5 After a prolonged infection with the disease causative agent, investigations
of coagulations tests revealed hypercoagulation. Discuss how the primary
diagnosis could have contributed to the hypercoagulable state in this patient. (10)
6
 |
7 Page 7 |
▲back to top |
9.6 What are the histological characteristics of this infection?
(4)
9.7 Name the technique specifically employed in histopathology to identify this
(1)
organism.
END OF QUESTION PAPER
7





